Our Work

Any maternal death is a travesty, and has wide-reaching negative consequences impacting on the health, education and financial stability of her family left behind. We target the United Nations’ Sustainable Development Goal 3.1 to reduce the global maternal mortality ratio to 70 by 2030. Our work seeks to directly reduce maternal mortality, by tackling all three of the critical delays described by Thaddeus, S. et al. (1994) that prevent women accessing timely reproductive healthcare (health education, access to healthcare and quality of care once accessed).
Antenatal Care
In line with WHO guidance, we aim to see our mothers six-weekly during their pregnancy at one of our permanent clinics. This aims to identify mothers at increased risk from complications, and also detect problems as they are arising, such that these issues can be dealt with in a timely and appropriate way. We offer health education on a variety of topics (see below) and in the antenatal period we offer prophylaxis for malaria (see below), worms and anaemia.
Between our two rural clinics in Runga and Kyarushesha we see in the region of 500 mothers each month for antenatal checks, in addition to those seen by our colleagues at Azur.
Intrapartum Care
Intrapartum care refers to that given to a mother during her labour and the birth of her baby. At both Runga and MAMA Grace Clinic in Kyarushesha we help mothers give birth to their babies safely, acknowledging that skilled birth attendance and health facility delivery are recognised as being two of the major contributors to reducing maternal mortality. If complications arise during childbirth in our rural clinics, we have a robust referral service to transport a mother, or a mother and her baby, to a higher level of care as required, for example if a caesarean section is needed, or if the baby is unwell after birth.
We aim to identify those mothers who are high risk during their pregnancy, through careful risk assessment at antenatal visits, and encourage these women to deliver in a facility offering access to a theatre in case of an emergency. This might be with our partners at Azur (non-governmental, not for profit), or at the local governmental hospital: Hoima Regional Referral Hospital.
Postnatal Care
We encourage mothers to stay in our clinics with their newborn baby for a minimum of 24 hours after birth to ensure that both mum and baby are well and that breastfeeding is well established. If there are concerns about infection, low birthweight or prematurity then we ask the mothers to stay with us for longer to complete treatment and ensure their baby is well before discharge home. Some babies will receive their basic immunisations prior to discharge, whereas others will be asked to return when the immunisation clinic is running, usually monthly.
If there are complications due to severe bleeding or preterm infant for example, then we will refer the mother and baby to a higher level of care in Hoima town.
High Dependency Care
In 2019 MAMA opened a two-bedded high dependency unit at Azur Health Centre. This is used by all the departments at the hospital, but most commonly for unwell mothers either during pregnancy or after delivery. To keep this staffed at all times we fund the salaries of two midwives at Azur Health Centre.
Neonatal Care
We support the Kangaroo Mother Care (KMC) unit at Azur Health Centre, as this is where premature or unwell babies are cared for following birth. Mothers are taught how to care for their infant, and nursing staff administers necessary treatment, which often includes oxygen therapy and antibiotics.
Malaria
In line with WHO guidance, we aim to see our mothers six-weekly during their pregnancy at one of our permanent clinics. This aims to identify mothers at increased risk from complications, and also detect problems as they are arising, such that these issues can be dealt with in a timely and appropriate way.
We offer health education on a variety of topics, including contraception, the WHO nine danger signs in pregnancy, and a safe place for delivery. During the antenatal period we offer prophylaxis for malaria (see below), worms and anaemia according to gestation.
Between our two rural clinics in Runga and Kyarushesha we see in the region of 500 mothers each month for antenatal checks, in addition to those seen by our colleagues at Azur.
Maternity Waiting Home (Runga)
We were very lucky to have two students from University of East Anglia fund raise and oversee the building of a small waiting home at our clinic in Runga in 2017. Often, especially in the rainy season, the marram roads and tracks can be very difficult to navigate and in particular travelling at night is unsafe. The waiting home means that mothers from neighbouring villages, who have further to travel to reach us to deliver their babies, have the option to stay with us for a few days and wait for the onset of labour.
Health Education
Health education talks are a very important part of the services offered by our clinics. Mostly, but not always, they take place during antenatal clinics, making it convenient for expectant mothers to attend. In order to target their husbands as well, we often take five minutes to speak during a weekly church service, or at times deliberately travel to a village to speak with the wider community. This is usually led by one of the Ugandan midwives we work with, but at times members of the community will speak about their experiences.
The topics vary depending what we have experienced recently in our clinics and also what the government recommend. Regular topics include the WHO nine danger signs in pregnancy; contraception; choosing a safe place for childbirth and the importance of health facility delivery and skilled birth attendance; and malaria prevention.
Family Planning
Reliable provision of contraception allows women to choose when they conceive, allows safe spacing of pregnancy (WHO recommends two years between delivery and conception) and can reduce transmission of sexually transmitted infections (STIs). Collectively these reduce both morbidity and mortality. Recent evidence suggests that uptake of contraception in Uganda remains low (17% of women of reproductive age, and 18% of married women).
Barrier methods of contraception are popular across communities in Uganda, and have the advantage of reducing transmission of STIs. However, their efficacy is lower than some other methods. All our staff members are trained in provision of long-acting reversible contraceptives, allowing us to offer the intrauterine contraceptive device (IUCD), Depo Provera and contraceptive implant. Contraceptive methods are provided free-of-charge by the Ugandan Protestant Medical Bureau (UPMB).
Other contraceptive methods sadly still carry myths around their use, especially within rural Uganda. Education about contraception is key for dispelling these and providing reliable information about the range of methods available. Often it is perceived that once a girl or woman is using contraception, they are automatically sexually active. Within Ugandan communities this frequently carries stigma. Contraceptive education addresses the benefits that contraception can have that are often not considered, alongside the clear benefits of reducing unwanted pregnancies and child spacing: these include lighter or no periods, scheduled bleeding, reduction of pain and mood stabilisation. These can all significantly improve the lives of women and girls, and are especially relevant when living in remote areas where access to sanitary provision can result in girls missing out on school or day-to-day activities.
Sexual Health
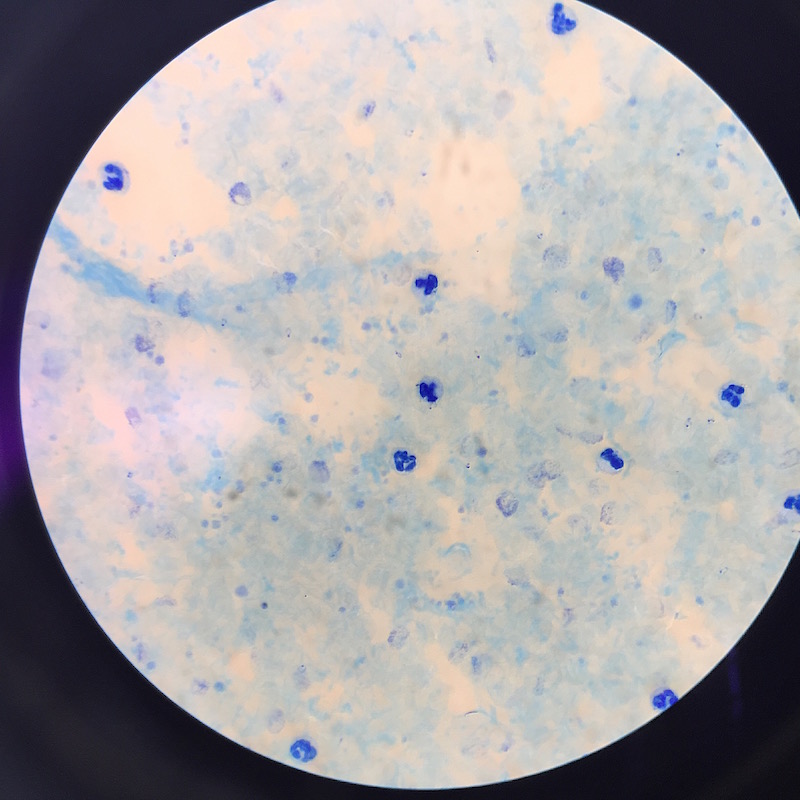
Our clinics provide health education and regular screening for HIV/AIDS and other sexually transmitted infections (STIs), assisting in the promotion of regular STI checks as part of routine healthcare. These checks need to become commonplace and part of everyone’s health priorities. We aim to reduce the stigma surrounding screening and diagnosis of HIV and other STIs. The mantra of ‘undetectable = un-transmittable’ will be promoted to encourage people to commence and maintain antiretroviral medication when HIV is diagnosed.
Our clinics screen all women for HIV and syphilis at their booking antenatal visit and then again in both the second and third trimesters, and postpartum. Any mothers diagnosed as HIV positive in pregnancy will be given counselling and support with partner notification and be provided with appropriate antiretroviral treatment. Follow up within the postnatal period is offered, plus treatment and testing for their baby especially if diagnosed late in pregnancy.
When syphilis is diagnosed, partner notification will be undertaken and the WHO recommended treatment guideline adhered to, in order to ensure cure.
Staff Training
Midwifery is “skilled, knowledgeable, and compassionate care for childbearing women, newborn infants, and families across the continuum throughout pregnancy, and the early weeks of life”. MAMA believes the midwives and staff in our clinics should be up to date with their skills and knowledge, not just through clinical experience, but also formal staff training days. Midwives have been identified as key players in, amongst other things, reducing maternal and neonatal mortality and morbidity, and a reduction in stillbirths and pre-term infants (Midwifery Series 1, Lancet 2014).
Programme for Accessible Health Communication and Education (PACE) is a Ugandan organisation, which travels nationally to offer updating courses, but only one or two midwives from each hospital are released for this and new information is not always passed onto those who were unable to attend. In the past MAMA conducted informal training as we worked alongside midwives; topics determined by what was happening in the unit at the time. Since December 2015, MAMA has provided annual mandatory training at Azur Health Centre to all the midwives employed by Azur Health Centre and the MAMA clinics. Presenters from both the UK and Uganda and the training days follow a similar format to those in the UK with presentations, skills and drills workshops, train the trainer programmes and breakout sessions to discuss topics in further detail. Subjects covered include management of pre-eclampsia and eclampsia; postpartum haemorrhage; sepsis; shoulder dystocia; breech; management of prolonged or obstructed labour; neonatal resuscitation; and safeguarding.
Projects
MAMA runs projects targeting key maternal health issues in Uganda, aligning with both Ugandan government and international priorities for the reduction of maternal deaths. By educating mothers, training staff and ensuring access to appropriate care, MAMA is working to achieve early diagnosis and intervention and reduce maternal morbidity and mortality. Haemorrhage remains the leading cause of maternal death in Uganda, with pre-eclampsia being the second and sepsis the third. We have targeted the first two conditions directly, and have aimed to improve infection control practices, especially in settings where water supply can be inconsistent, by introducing home made hand gel.

Hand Gel
After fundraising themselves to support the project, Charlotte and Lucy Kirkpatrick spent a month in Hoima, in July 2019, making sanitising hand gel and sharing this skill with our Ugandan colleagues. The project has now been taken over by one of our wonderful midwives, Eunice, and William, our superb nurse colleague who works in paediatrics at Azur.

Pre-eclampsia / Eclampsia
In October 2017 MAMA conducted a health project about pre-eclampsia (PET) and eclampsia, which was delivered to staff and women in 31 health centres around the Hoima District. To staff we gave some updated information and training on diagnosis and management, as well as giving each health centre a well-stocked emergency box to manage the condition. For women we delivered health education talks about the danger signs of pre-eclampsia and eclampsia, and when to seek help.
Postpartum Haemorrhage
Due to the success of the PET project in 2017, in May 2018 we repeated the exercise but this time focussing on postpartum haemorrhage (PPH). We provided each health centre with an emergency box stocked with drugs and equipment for managing haemorrhage, and again addressed the women about danger signs and when to seek help. Women who were identified, during pregnancy, as high risk for PPH were advised to deliver at a facility where such an emergency could be managed by a team of health workers rather than in the village. It was great to see the same health centres using the PET boxes we had delivered 6 months before.